The Principles, Potential, and Pitfalls of Cold Therapy: A Review
Seemingly everywhere you look these days, somebody is taking a cold plunge and raving about the energy boosting, mood enhancing, and muscle recovering effects. The market for at home and wellness center cold plunges is taking off.
Is the rage about cold plunging really worth it? Does deliberate cold exposure have any scientifically validated staying power for your health and fitness routine? Or is it just the next fad in an endless series of wellness trends and hacks that are here today and gone tomorrow?
In order to provide a proper prescription for the use of deliberate cold exposure, we must drill down into the physiological effects of a cold stimulus on our bodies, examine the current data on the performance and health effects of cold therapy, and address certain limitations and outstanding considerations. First, however, let’s level set on the different modalities of cold therapy and their respective representation in the current scientific literature.
Modalities of Cold Therapy
The practice of deliberate cold exposure has been around for millennia. But recent adaptations include ice baths, brisk daily showers, outdoor swims, cold water immersion therapy, and cryotherapy sessions.
The majority of research to date comes from studies using cold water immersion (CWI) which is perhaps the most controllable method of cold therapy. CWI has been defined as submersion to the neck in water temperatures of less than 15°C (59 degrees Fahrenheit); however, primary research studies have employed lower temperatures between 8°C and 10°C, with others lowering water to 5°C.
Cryotherapy –or whole-body cryotherapy (WBC), more specifically—is a newer form of deliberate cold exposure that entails exposing the body to subzero temperatures (as cold as -200 degrees Fahrenheit) in a special tank or chamber for 2 to 4 minutes.
The cold stimulus in WBC is produced by liquid nitrogen, a gas, whereas CWI uses water, a liquid. CWI and WBC can both apply a cold stimulus to elicit an involuntary physiological response from cooling. Cooling occurs with a transfer of heat energy, which relies on thermal conductivity. Thermal conductivity depends on various factors but largely the heat transfer coefficient. This coefficient is much smaller for air-WBC (0.0024) compared to water-CWI (0.58). Hence, even though the WBC air temperature is much colder than the water temperature in CWI, the water has far greater thermal conductivity. A study from Costello and colleagues found comparable reductions in muscle, skin and core temperature following after 4 minutes of exposure to either WBC -110°C or CWI to 46°F/ 8°C.
It is important to note that given the relatively recent advent of WBC, most of the research on deliberate cold exposure comes from studying the effects of CWI on human subjects. Existing studies employing WBC are sparse, and much less well designed.
Acute Physiological Response to a Cold Stimulus
Exposure to extreme cold acts as an acute stress that challenges the body’s physiological processes to maintain temperature homeostasis. After registering cold via temperature receptors in the skin, the body injects a robust surge of catecholamines—noradrenaline (aka norepinephrine) specifically—into the bloodstream, as mediated by the sympathetic nervous system. This stress response triggers the flight or fight mode, which causes increased alertness and focus, elevated heart rate, and more rapid breathing.
In order to maintain core body temperature, the blood vessels closer to the outside of the body constrict to keep blood focused on our internal organs and mitigate dissipation of heat through the skin. When the body’s core temperature falls below a critical threshold, it is unable to preserve heat by vasomotor control alone. As a second line of defense from heat loss, the skeletal muscles start shivering in order to generate heat. This increased muscle activity is highly energy dependent and hence, necessitates an elevated metabolic rate to generate heat. In addition, extreme and sustained cold may activate what is known as non-shivering thermogenesis. The cold exposure activates the uncoupling protein 1 (UCP1), which forces the mitochondria to produce heat, rather than ATP, from nearby fat stores. With repeated cold exposure, your adipose (fat) cells also compensate by increasing mitochondrial activity in adipose tissue.In cold conditions, this so-called brown adipose tissue or BAT burns fat to create heat that maintains core body temperature. Repeated cold exposure increases the capacity for non-shivering thermogenesis via BAT activation, which increases total daily energy expenditure..
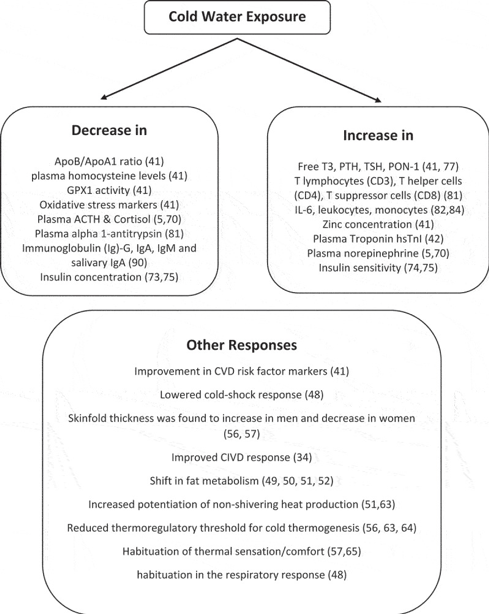
In a comprehensive review on the health effects of voluntary exposure to cold water, Espeland and colleagues summarize the acute effects of cold exposure on human physiology.
At a cellular level, extreme cold may slightly increase immune activity. White blood cells, which fight infection, circulate in your body more quickly when you are exposed to cold temperatures. Regular exposure to cold may also help your immune system produce more cytokines and white blood cells to counter regular inflammatory stresses.
On a biochemical or molecular level, cold exposure triggers an increase in free-radical production, and a corresponding decrease in antioxidant levels to counter this oxidative stress. Over time with repeated cold exposure, the body may actually compensate by increasing the baseline concentration of antioxidants like activated glutathione.
Evidence shows that cold exposure may also release brain chemicals like dopamine which is responsible for motivation and reward. Dopamine enhances focus and attention, elevates mood, and promotes goal directed behavior.
Preliminary evidence shows that cold exposure in air or water increases the production of adiponectin—a protein that plays an important role in protecting against insulin resistance, diabetes, atherosclerosis and other age-related diseases—in adipose tissue through the process of shivering and non-shivering thermogenesis. And repeated cold-water immersions during the winter months has been shown to significantly increase insulin sensitivity and decrease insulin concentrations.
Cold exposure upregulates the activation of genes involved in lipid metabolism (fat burning) and the group of proteins known as cold shock proteins, such as RNA-binding protein 3 (RBM3) and cold-inducible-RNA-binding protein (CIRP). Preliminary evidence from animal studies suggests that these proteins help protect neurons in the brain from damage and act as antioxidants to protect against cell death from oxidative stress and free radical damage. Cold-shock proteins may also be involved in muscle repair and the preservation of muscle mass.
Chronic Physiologic Adaptation of Repeat Cold Stimulus
The physiological changes above characterize the immediate, short term impact of a cold stimulus on the body. To date there is no direct causal evidence for the role of repeated, deliberate cold exposure in the prevention or treatment of disease. It seems mechanistically plausible, with some supportive associative evidence, that over time, repeated or chronic cold exposure attenuates these changes and produces “hardening”—an increased tolerance to unforeseen external stress, such as disease.
Espeland and colleagues summarize and cite evidence for wide-ranging physiological adaptations to repeated cold-water exposure. It should be noted, however, that these findings, particularly the effect of CWI on the body’s hormonal systems, are preliminary in nature with little, and at times conflicting data.
Performance Effects of Cold Therapy
Regular and repeated cold exposure seems to confer an adaptive, increased tolerance to stress as evidenced by increased concentrations of antioxidants. Young men exposed to cryotherapy for 3 minutes at 202°F (−130°C) every day for 20 days doubled the activity of one of the most potent antioxidant enzyme systems in the body called glutathione reductase and increased another potent antioxidant enzyme called superoxide dismutase by ~43%. Elite kayakers that engaged in whole body cryotherapy (248 to 284°F or 120 to 140°C) 3 minutes a day for 10 days increased the activity of superoxide dismutase by 36% and glutathione peroxidase by 68%.
The utility of cold therapy prior to athletic training to eliciting favorable physical and physiological responses is currently unclear with a paucity of good quality research.
There has been more investigation of the use of cold exposure as a recovery tool for physical training based on the mechanistic plausibility that cold temperature reduces swelling, inflammation, and tissue breakdown. As a recovery tool following high intensity exercise (mainly running and athletic training), the existing literature, as reviewed in a comprehensive meta-analysis, shows that cold-water immersion is more likely to positively influence muscular power performance, muscle soreness, serum creatine kinase, and perceived recovery in the short term. Cold water immersion at lower temperatures and for shorter durations (i.e. <12mins) may be more effective for quick recovery, especially if you need to perform repeatedly over a short time span. . However, use of cold therapy is not positively adaptive, and may even be counterproductive in the long term, and particularly for physical training that targets strength and hypertrophy adaptations. There have been some studies showing decreased long term gains in muscle mass and strength with repeated cold immersion, perhaps by blunting the activation of key proteins and satellite cells needed for skeletal muscle adaptations.
Recent claims have also been made about cold stimulation and the direct effect on the nervous system, particularly measured by improved heart rate variability (HRV). It is hypothesized that cold immersion may improve (increase) HRV, by stimulating the vagus nerve which can directly impact the parasympathetic nervous system. However, the data in humans is limited. Using cold stimulation at the neck, Jungmann and colleagues demonstrated an increase in HRV and a reduction in resting heart rate, suggesting a stimulation of cardiac-vagal activation. However, in a study examining both short and long term effects of cold water immersion on young fit cyclists, HRV benefits were only seen in the minutes after cold exposure. Four hours later, all effects were gone. This seems to be the case for long term cold exposure as well. Stanley and colleagues examined regular CWI on HRV after long term exercise, and although exposure appeared to help cycling time trial consistency after several days of training, vagal-HRV varied over time and depended more on prior exercise intensity. Interestingly, however, a recent study in runners showed that CWI after an intense bout of exercise increased HRV during sleep, which may have affected recovery by improving sleep quality.
Health Impact of Cold Therapy
Cold exposure is commonly used as a therapeutic tool for musculoskeletal healing and management of chronic pain. Noradrenaline and beta-endorphins are endogenous pain suppressors, which likely explains why cold exposure can act as an analgesic. In patients with osteoarthritis, whole-body cryotherapy has been shown to reduce the frequency and degree of pain perception and decrease reliance on analgesic medications; it improved the range of physical activity and had a positive effect on their overall well-being. In patients with systemic inflammatory conditions, such as rheumatoid arthritis, 10-day comprehensive therapies including different local cryotherapies for the patients with RA cause significant decrease in TNF-α systemic levels, meaningfully improve DAS28, HAQ scores, and some functional parameters, but do not change IL-6 levels. Some, albeit limited, suggests effectiveness of cryogenic temperature interventions in inflammatory conditions like ankylosing spondylitis, fibromyalgia, multiple sclerosis, and chronic low back pain.
In terms of metabolic health, repeated intermittent cold exposure has been shown to both increase brown adipose tissue (BAT) and increase BAT Activation in animal models. Preliminary data in humans shows increased BAT activation in parallel with an increase in nonshivering thermogenesis with repeated cold exposure. The production of heat requires the expenditure of energy. In cold environments, the body must produce more heat to maintain its temperature, thus burning more calories. To date, few human trials exist that tested the effect of cold exposure on BAT; these studies show that BAT, activated by beta adrenergic receptors, contributes a small yet highly variable amount to overall energy expenditure. Given that BAT deposits in humans are only a few grams, BAT contributes a small amount to overall energy metabolism which is unlikely to cause weight loss. There is no convincing evidence yet to indicate that BAT may be a viable pharmaceutical target for body weight loss or even weight loss maintenance. Although the role of BAT in weight control is currently unsubstantiated, BAT may play a role in improving insulin sensitivity in humans. Activating BAT and inducing browning of white adipose tissue can accelerate the intake of glycolipids and reduce the insulin secretion requirement.
The known increases in noradrenaline, beta-endorphin and dopamine due to a cold stimulus may have a positive effect on mental health and brain development. To date, however, there is no clinical evidence (other than case reports) that cold exposure can improve brain health or treat mental health conditions. The positive mental health aspect of regular winter swimmers is mostly based on questionnaires and anecdotal evidence. That said, researchers are exploring the psychological effects of cold water exposure and have seen encouraging results on mood. And there is preliminary data to suggest that whole body cryotherapy can be a useful adjunctive therapy for depressive symptoms and anxiety disorders. Perhaps WBC may even increase the performance of cognitive functions in patients with early MCI.
Lastly, there is anecdotal evidence that winter swimmers are more resistant to infectious illnesses, which implicates cold water immersion in immune health. However, the evidence is sparse and conflicting. One clinical study of upper respiratory tract infections in cold-water swimmers compared to pool swimmers found no significant difference in the prevalence of these infections. Another found an association between winter swimming and a 40% decreased incidence of respiratory tract infections.
Safety, Efficacy, and Effectiveness Considerations of Cold Therapy
Deliberate cold exposure is generally a safe endeavor. The most prevalent risks are related to cardiorespiratory problems that are often related to the initial cold shock when entering cold. In particular, the initial shock of plunging into icy water can trigger arrhythmias and heart attacks, likely due to conflicting sympathetic and parasympathetic inputs. And even though we are discussing deliberate (and presumably controlled) cold exposure here, it would be remiss to not mention risk of hypothermia and its well-known consequences. For cryotherapy specifically, the main risks are frostbite and burns to the skin if the extremities are not properly covered.
Determining the efficacy of all of the techniques and practices of deliberate cold exposure is challenged by existing data, which is limited in both quality and quantity. Many of the proclaimed health benefits are based on subjective claims and anecdotal cases. For cold water immersion and newer modalities like cryotherapy, studies have small sample sizes, short durations and heterogenous study populations and exposure protocols. When body fatness and surface area to volume ratio are taken into account, there appears to be no major differences in thermosensitivity and metabolic heat production between men and women during cold water immersion. However, other physiological responses may differ between genders. And with advancing age, our bodies capacity for thermoregulation may decline, making us more susceptible to heat loss with cold exposure.
It will be challenging to tease out the impact of the cold stimulus directly in research on the impact of cold exposure. First, we cannot blind research participants to cold exposure to control for the powerful placebo effects. And most of the research to date involves cold water immersion or swimming which often comes hand in hand with numerous additional confounders including exercising, socializing, and spending time outdoors, all of which positively impact wellbeing. Additionally, the transition between acute and chronic adaptation to cold stress is unclear, which challenges proper protocol design and “dosing.”
Despite abundant anecdotal claims, the health claims for cryotherapy have not been the subject of well-designed studies. To date, there is no convincing evidence that that WBC effectively treats chronic pain conditions, causes weight loss, manages depression, improves recovery, or any of the other abundant health claims made by many gyms, spas, and wellness centers. The FDA has not cleared or approved WBC devices as safe and effective to treat medical conditions. However, some of the positive preliminary evidence indicates that currently there is an absence of evidence (as opposed to evidence of absence) for this modern cold exposure modality.
The Bottom Line: A practical application of cold therapy
There is truth in the adage “that which does not kill you only makes you stronger.” Cold therapy, if employed strategically like other acute stresses such as intense exercise, can provide an adaptive stimulus for the body. Meaning the body will compensate by increasing the cellular and biochemical mechanisms needed to regain homeostasis and better handle this stress in the future. Presumably the body develops enhanced resilience to better manage and cope with unforeseen stressors in other parts of life as well. The hypothesis that adapting to the shock of cold water may improve a person’s ability to handle other life stressors seems both plausible and promising.
Like any other deliberate stressor, the most effective stimulus will be appropriately targeted, timed, and tempered based on therapeutic goals. Currently, there are no standardized protocols for cold exposure mapped to specific need states or goals. Given the evidence to date, here are some basic concepts and biologically based suggestions for advantageous use:
If you are tired, unfocused, and feeling sluggish, a strong dose of cold therapy can be a great pick-me-up to enhance your energy, mood, and productivity. But do not trade off cold therapy for sleep. That would be majoring in the minors of health and wellness.
If cold is being used to enhance recovery and ease muscle soreness, your use of cold therapy would depend on your training goals. If you are an endurance athlete or in a competition that requires quick recovery, using cold therapy immediately after physical activity is a productive strategy. However, if you are primarily focused on muscular strength and hypertrophy, you would not want to employ cold exposure during post-training window where it would blunt or attenuate the inflammatory response, which is an essential stimulus for the adaptive response.
If regular cold exposure was being used to reduce pain from more chronic inflammation, you would want to employ this when inflammation is at its peak.
Do not expect cold therapy to be a solo solution to significant or sustainable weight loss. Given that BAT is such a small percentage of human adult mass, its overall contribution to energy expenditure is likely quite small for human adults. The increase in energy expenditure during cold exposure is predominantly driven by the shivering of muscle mass. Your resting metabolic rate would increase much more by moving your muscles by directly exercising them—consistently, vigorously, and against load.
If cold therapy helps ease your pain, lessen your depression, or better regulate your blood sugar, by all means use it! But do so safely and as part of a comprehensive treatment plan—not a standalone solution.